PRESS RELEASE
20 SEPTEMBER 2013
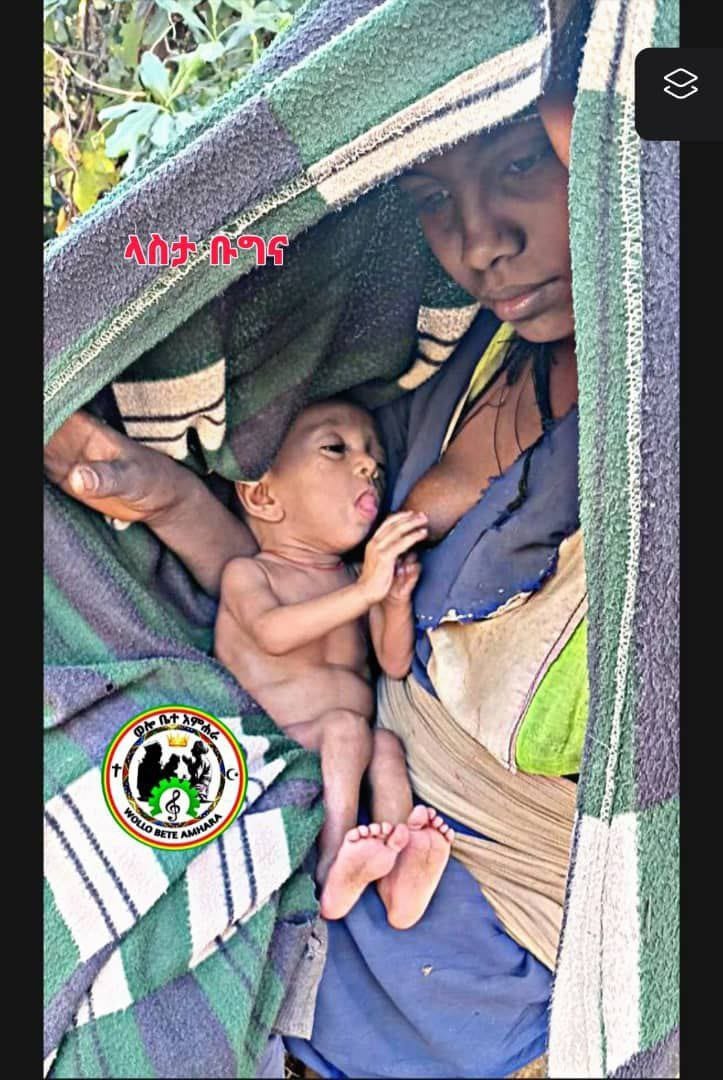
London — The UK support to the Global Fund is helping to bring healthcare to the doorstep of rural Ethiopians through the training and deployment of health extension workers.
While women continue to bear the brunt of health problems globally, many women are leading the way – inspiring improvements in healthcare and saving lives.
Abinet, 18, a farmer from a small community in Ethiopia believes he contracted tuberculosis (TB) from a friend whilst living in the city. “At the beginning, I thought it was just a common cold but I had a very serious cough. I couldn’t sleep late at night,” explains Abinet.
Ethiopia is one of 22 high-burden countries for TB and the disease is one of the main causes of morbidity and mortality. Initially, Abinet relied on traditional medicine, but his health didn’t improve and only got worse. This made him attend his local health centre.
“When I was very sick at the beginning, I had to be helped to the clinic. I could not walk there on my own. I had to sit and rest on the road because I was weak,” says Abinet.
The health centre is managed by Workalem Haile, 28, a local woman trained as a Health Extension Worker (HEW) through a programme supported by the Global Fund and the UK government. In total the programme has trained 37,000 HEWs across the country.
Workalem ensured Abinet was tested for TB, and when the results came back as positive he was prescribed the necessary medication. During the 6 months it took for Abinet to recover, Workalem visited his home regularly to make sure he continued to take his medication.
“My health has improved because of Workalem’s help. I would like to thank her very much,” says Abinet.
Taking the lead in health
For Workalem, the case of Abinet reflects a typical day as a HEW. Both Workalem and her colleague Misrach are responsible for the health centre in the village of Chama Hembecho, overseeing health services for over 2,200 families. Due to their hard work and dedication, there has been remarkable progress, particularly in children’s immunisation, hygiene and family planning.
“If my community can change, then so can I” says Workalem.
As a result of her work in the village, Workalem has gained a huge amount of respect and has been selected to serve on the Kebele (village) cabinet. “My hope is that people learn from me and change their lifestyle and remain free from disease,” asserts Workalem.
Fact and stats
Ethiopia’s 85 million inhabitants mainly live in small rural communities spread across mountains, making access to healthcare a challenge. However, in the last decade the Ethiopian government has built or upgraded 15,000 health facilities across the country. The results are remarkable, at present more than 92% of the population lives within 10km of a public health clinic.
The TB project is now delivering additional training to HEWs to provide TB detection and management services to their communities. Many TB sufferers are often too ill to make the short journey to their local health centre and women face cultural and geographical barriers. With their new skills, the HEWs can now collect saliva swabs directly from individuals during their door-to-door community visits and send them to laboratories.
The results are positive, TB diagnostic and treatment services have become more accessible to the poor, specifically women, elderly and children. Notification rates have doubled and a significant improvement in treatment outcomes can be seen, in 2011 the success rate reached 90%.
The TB REACH project has now been expanded to four additional zones and further scale-up is being planned by the national TB program.
SOURCE UK Department for International Development